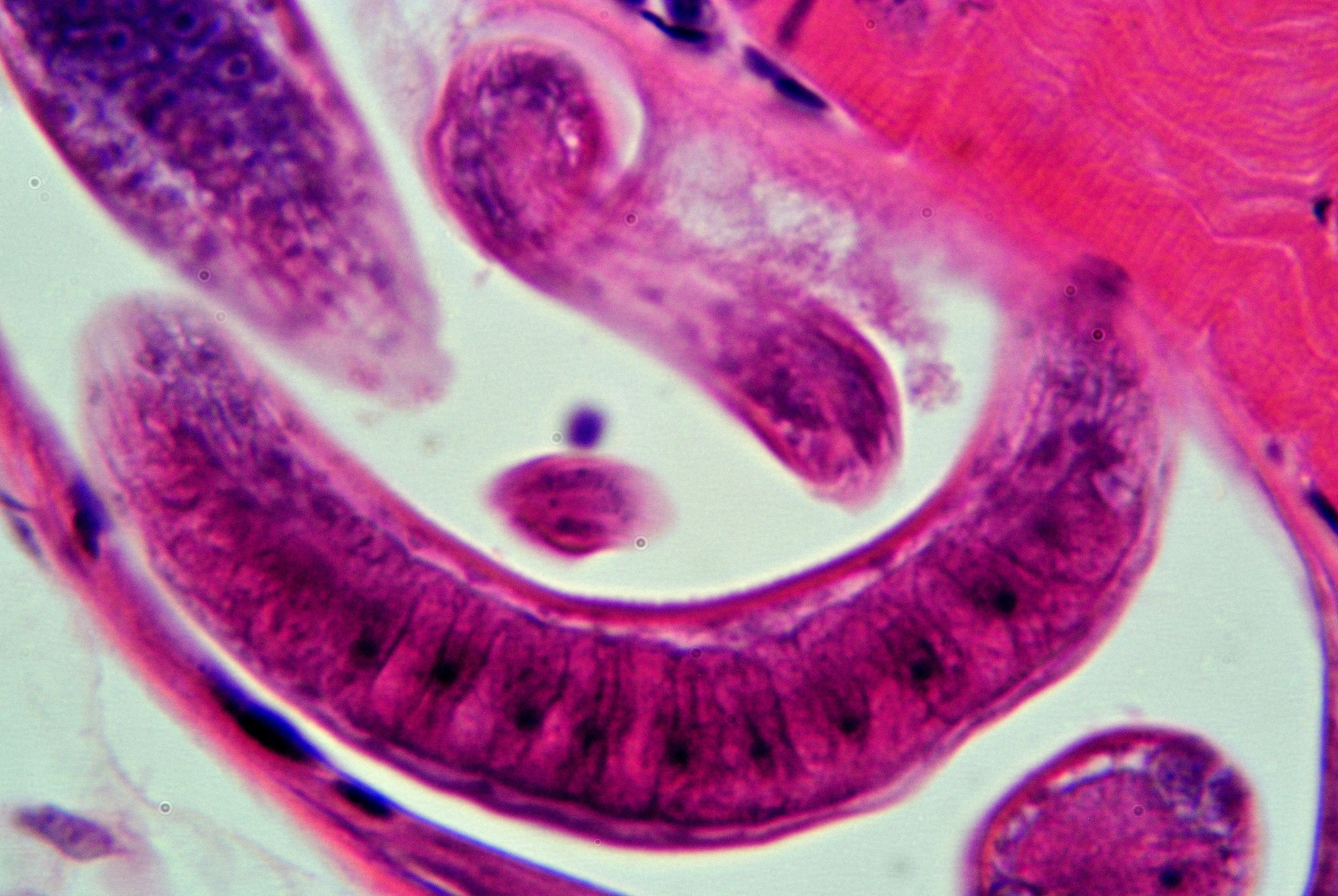
Trichinellosis is a parasitic disease of public health importance caused by the nematode of the genus Trichinella. Human infections are established by consumption of insufficiently cooked infected meat, usually pork or game meat, although other species have been implicated. Natural infections are found in wild carnivores; trichinellosis has also been found in horses, rats, beavers, opossums, walruses, whales, and meat-eating birds. Most mammals are susceptible. The number of human cases has declined in the past 50 years due in part to the move to modern production facilities (confinement) that reduces or eliminates exposure to rodents and other wildlife.
Trichinellosis is a serious disease of humans. It is estimated that there are likely ten thousand human infections per year worldwide.
The symptoms depend on the stage of the infection. Initially when larvae or adults are in the intestines there may be abdominal discomfort with nausea, diarrhea, vomiting, fatigue, fever, and abdominal discomfort.
As larvae migrate into the muscles, they may cause severe pain, headaches, fevers, chills, cough, eye swelling, aching joints and muscle pains, itchy skin, rash, and diarrhea or constipation. The severity of the disease is related to the number of larvae ingested, and fatalities can occur with high doses.
In most developed countries where trichinellosis has been controlled in domestic pigs, human infection is more likely from eating game or horse meat. However, the majority of cases in the world are still caused by eating insufficiently cooked meat from domestic swine and wild boar.
Trichinellosis is a zoonosis with a worldwide occurrence and endemic in most part of Asian, even some pacific island counties. The genus Trichinella is currently considered a complex of nine species and three additional genotypes.
The parasite has also been shown to be endemic in Cambodia, Indonesia, Lao PDR, Malaysia, Myanmar, and Papua New Guinea either in humans or in animal hosts [1]. Trichinellosis is among the most common food-borne parasitic zoonoses in Thailand and many outbreaks were reported each year [2,3,4]. Trichinella is also circulating in the domestic life cycle in northwestern Vietnam [5,6].
In P.R.China, the trichinella species that have been reported are T. spiralis (mainly infected pigs) and T. nativa (mainly infected dogs) [7]. Aside from T. spiralis and T. nativa, T. pseudospiralis, and T. papuae infections have also been reported in Chinese Taipei as a result of ingesting raw soft-shelled turtles [8]. In Japan, an epidemiological investigation from 2003 to 2006 showed T. nativa and Trichinella. T9 were found in many species of wildlife such as foxes, raccoons and brown bears [9,10]. In Korea RO, a human infection by T. spiralis in 1997 was confirmed by the consumption of raw badger meat and other several cases were related with the raw wild boar meat [11].
In Iran, Trichinella have mainly been detected in carnivorous mammals. T. murrelli mainly occurrence in the wild boar host [12,13].
In Asia and the Pacific region, the OIE Collaborating Center for Foodborne Parasites is located in Jilin University, P.R.China. This center has the independent capabilities and skills to perform diagnostic tests and characterization for parasites transmitted by food: Helminthes (Trichinella, Taenia solium, Fascioliasis), Protozoa (Toxoplasma, Cryptopsoridium). It also works to develop new diagnostic methods and produces reference reagents; it can provide training, expertise, scientific and technical support to laboratories in this field for region Members if necessary; it can also provide advices on national or regional control policies as well as related educational activities.
OIE is also addressing other food safety related issues and collaborating with FAO and WHO to promote multi-sectoral approach to control and prevent foodborne and zoonotic parasitic diseases.
Reference
1: Pozio E. New patterns of Trichinella infection. Vet Parasitol. 2001 Jul 12;98(1-3):133-48. doi: 10.1016/s0304-4017(01)00427-7.
2: Kaewpitoon N, Kaewpitoon SJ, Pengsaa P. Food-borne parasitic zoonosis: distribution of trichinosis in Thailand. World J Gastroenterol. 2008 Jun 14;14(22):3471-5. doi: 10.3748/wjg.14.3471.
3: Kusolsuk T, Kamonrattanakun S, Wesanonthawech A, Dekumyoy P, Thaenkham U, Yoonuan T, Nuamtanong S, Sa-Nguankiat S, Pubampen S, Maipanich W, Panitchakit J, Marucci G, Pozio E, Waikagul J. The second outbreak of trichinellosis caused by Trichinella papuae in Thailand. Trans R Soc Trop Med Hyg. 2010 Jun;104(6):433-7. doi: 10.1016/j.trstmh.2009.12.005.
4: Intapan PM, Chotmongkol V, Tantrawatpan C, Sanpool O, Morakote N, Maleewong W. Molecular identification of Trichinella papuae from a Thai patient with imported trichinellosis. Am J Trop Med Hyg. 2011 Jun;84(6):994-7. doi: 10.4269/ajtmh.2011.10-0675.
5: Thi NV, De NV, Praet N, Claes L, Gabriël S, Dorny P. Seroprevalence of trichinellosis in domestic animals in northwestern Vietnam. Vet Parasitol. 2013 Mar 31;193(1-3):200-5. doi: 10.1016/j.vetpar.2012.11.023.
6: Vu Thi N, Dorny P, La Rosa G, To Long T, Nguyen Van C, Pozio E. High prevalence of anti-Trichinella IgG in domestic pigs of the Son La province, Vietnam. Vet Parasitol. 2010 Feb 26;168(1-2):136-40. doi: 10.1016/j.vetpar.2009.10.024.
7: Bai X, Hu X, Liu X, Tang B, Liu M.Current Research of Trichinellosis in China. Front Microbiol. 2017Aug 2;8:1472. doi: 10.3389/fmicb.2017.01472. eCollection 2017.
8: Lo YC, Hung CC, Lai CS, Wu Z, Nagano I, Maeda T, Takahashi Y, Chiu CH, Shyong Jiang DD. Human trichinosis after consumption of soft-shelled turtles, Taiwan. Emerg Infect Dis. 2009 Dec;15(12):2056-8. doi: 10.3201/eid1512.090619.
9: Kanai Y, Inoue T, Mano T, Nonaka N, Katakura K, Oku Y. Epizootiological survey of Trichinella spp. infection in carnivores, rodents and insectivores in Hokkaido, Japan. Jpn J Vet Res. 2007 Feb;54(4):175-82.
10: Kobayashi T, Kanai Y, Ono Y, Matoba Y, Suzuki K, Okamoto M, Taniyama H, Yagi K, Oku Y, Katakura K, Asakawa M. Epidemiology, histopathology, and muscle distribution of Trichinella T9 in feral raccoons (Procyon lotor) and wildlife of Japan. Parasitol Res. 2007 May;100(6):1287-91. doi: 10.1007/s00436-006-0402-x.
11: Kim G, Choi MH, Kim JH, Kang YM, Jeon HJ, Jung Y, Lee MJ, Oh MD. An outbreak of trichinellosis with detection of Trichinella larvae in leftover wild boar meat. J Korean Med Sci. 2011 Dec;26(12):1630-3. doi: 10.3346/jkms.2011.26.12.1630.
12: Mowlavi G, Marucci G, Mobedi I, Zahabiioon F, Mirjalali H, Pozio E. Trichinella britovi in a leopard (Panthera pardus saxicolor) in Iran. Vet Parasitol. 2009 Oct 14;164(2-4):350-2. doi: 10.1016/j.vetpar.2009.05.001.
13: Kia EB, Meamar AR, Zahabiun F, Mirhendi H. The first occurrence of Trichinella murrelli in wild boar in Iran and a review of Iranian trichinellosis. J Helminthol. 2009 Dec;83(4):399-402. doi: 10.1017/S0022149X09990319.